Abstract
Background: Individuals with chronic kidney disease (CKD) are at exceptionally high risk of both thrombosis and bleeding events. Limited comparative effectiveness evidence exists regarding the optimal choice of thromboprophylaxis in those with CKD. We set out to compare the safety and effectiveness of direct oral anticoagulants (DOACs) versus low-molecular-weight heparin (LMWH) among older individuals with CKD following hip or knee arthroplasty.
Objective: To assess the 90-day risk of a venous thromboembolism (VTE) or hemorrhage with DOAC use compared to LWMH after hip or knee arthroplasty among older individuals with CKD.
Methods: A population-based, retrospective cohort study was conducted among adults of age ≥ 66 with CKD undergoing hip or knee arthroplasty who had filled an outpatient DOAC prescription (apixaban, rivaroxaban, dabigatran, edoxaban) after surgery compared to LMWH (enoxaparin, dalteparin, tinzaparin) between January 1, 2010 and December 31, 2020 in Ontario, Canada. CKD was defined by at least one estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73 m2 within 2 years or the presence of chronic dialysis within 5 years. Index was the date of first filling of the outpatient anticoagulant prescription after hip or knee arthroplasty. The primary effectiveness outcome was VTE and the primary safety outcome was any hemorrhage identified by validated algorithms using relevant diagnosis and billing codes. Patients were followed until 90 days after index, end of Ontario insurance, death, or the end of follow-up period on March 31, 2021. Overlap weighted cause-specific Cox proportional hazard models were used to examine the association of the 90-day risk of a VTE and/or a hemorrhage event accounting death as a competing risk. In additional analyses, we examined a more stringent VTE defining algorithm (diagnostic codes plus procedure codes within 7 days), different eGFR cut-offs, limiting to the most commonly used DOAC and LWMH (rivaroxaban vs. enoxaparin), and a shorter (30-day) follow up period.
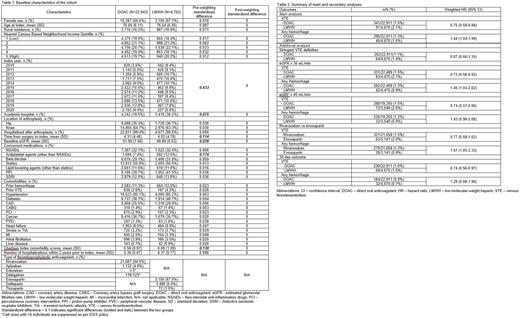
Results: A total of 27,645 patients were prescribed DOAC or LMWH after arthroplasty (66.7% female, mean age 76, DOAC: 22,943, LMWH: 4,702, mean eGFR 51.6 mL/min, 17.7% with eGFR < 45 mL/min). DOAC users had higher eGFRs, less comorbidity, had surgeries in more recent years, were more likely to be treated in community hospitals, and with shorter time from surgery to index compared to LMWH users (Table 1). After accounting for multiple covariates, the use of DOAC, compared to LMWH, was associated with less VTE events (DOAC: 341/22,943 [1.5%] vs LMWH: 97/4,702 [2.1%], weighted hazard ratio [wHR] 0.75, 95% confidence interval [CI] 0.59-0.94) and more hemorrhage events (DOAC: 290/22,943 [1.3%] vs LMWH: 45/4,702 [1.0%], wHR 1.44, 95% CI 1.04-1.99) (Table 2)]. The findings were consistent in all additional analyses (Table 2).
Conclusions: Among older adults with CKD, DOAC use was associated with lower VTE and higher hemorrhage risk compared to LMWH following knee or hip arthroplasty.
Disclosures
Wang:Servier: Other: Advisory board; Leo Pharma: Research Funding; Valeo: Other: Advisory board. Sood:AstraZeneca: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.